Blurred vision after cataract surgery? Posterior capsular opacification is treatable. A quick, painless YAG laser capsulotomy restores clear vision, improving daily life instantly.
What is a Secondary Cataract?
A secondary cataract, medically known as posterior capsular opacification (PCO), is a common complication that can occur after cataract surgery. It is not a true cataract but a clouding of the posterior capsule, the part of the eye that holds the artificial lens implanted during the surgery.
During cataract surgery, the natural lens of the eye is removed, leaving the posterior capsule intact to support the new artificial lens. Over time, this capsule may become cloudy due to the migration and proliferation of residual lens epithelial cells.
This condition can lead to symptoms similar to the original cataract, such as blurred vision, glare, and difficulty seeing clearly, even though the artificial lens remains clear. PCO typically develops weeks to months after surgery, but in some cases, it may take years to appear.
Fortunately, posterior capsular opacification is treatable with a simple, outpatient procedure called a YAG laser capsulotomy, which restores clear vision.
Causes of posterior capsule opacification
Posterior capsule opacification occurs due to biological changes following cataract surgery. Although the surgery replaces the cloudy lens, the natural capsule that holds the artificial lens remains in place. Over time, the following processes can lead to PCO:
Residual Lens Epithelial Cells (LECs):
During cataract surgery, not all lens epithelial cells can be removed.
These residual cells migrate and multiply on the posterior capsule, leading to clouding.
Fibrosis:
Some lens epithelial cells differentiate into fibroblast-like cells.
This causes the capsule to thicken and become opaque, impairing light transmission.
Proliferation and Migration:
Lens cells may grow over the capsule, forming a cloudy membrane.
This process is influenced by healing responses and individual biological factors.
Inflammatory Response:
Mild inflammation after surgery can contribute to the activation of lens epithelial cells.
These processes are part of the body’s natural healing mechanism, but they result in the opacification of the posterior capsule over time.
What are the symptoms of posterior capsular opacification (PCO)?
Posterior capsular opacification (PCO) can develop after cataract surgery and may affect vision. Common symptoms include:
Blurry or Hazy Vision: Patients often describe their vision as cloudy or foggy, similar to the symptoms of cataracts.
Glare and Halos: Increased sensitivity to bright lights, often accompanied by glare or halos, especially in low-light conditions.
Decreased Visual Acuity: A gradual decline in sharpness or clarity of vision.
Difficulty Reading or Seeing Details: Challenges with activities that require fine vision, such as reading or recognizing faces.
Reduced Contrast Sensitivity: Colors and contrasts may appear duller, making objects less distinct.
These symptoms can vary in severity depending on the extent of the opacification. If untreated, they may worsen over time, impacting daily activities.
How long after cataract surgery can posterior capsular opacification occur?
Posterior capsular opacification can appear at different times after cataract surgery. It often develops within weeks or months as the healing process begins. In some cases, it may take years to occur. Symptoms usually start gradually and worsen over time.
Younger patients and those with certain eye conditions or surgical complications have a higher risk of early onset. Regular eye exams after cataract surgery help detect PCO early. Early treatment prevents symptoms from affecting daily life.
How posterior capsular opacification affects daily activities?
Posterior capsular opacification (PCO) can significantly impact daily life by reducing the quality of vision. This impairment can make routine tasks challenging, including:
Reading: The clouded vision caused by PCO can make it difficult to read books, newspapers, or electronic screens.
Driving: Blurred vision, glare, and halos, particularly at night, can make driving unsafe.
Working: Tasks requiring detailed focus, such as using a computer, may become frustrating and inefficient.
Social Interaction: Difficulty recognizing faces or reading body language can hinder communication.
Household Tasks: Activities like cooking, cleaning, or sewing may require additional effort and pose safety risks.
Outdoor Activities: Increased sensitivity to light can make outdoor activities uncomfortable, especially in bright sunlight.
The progressive nature of PCO may lead to a loss of independence over time, underscoring the importance of timely diagnosis and treatment.
Comparing posterior vs secondary cataract symptoms
Posterior capsular opacification (PCO) develops after cataract surgery, while a posterior cataract refers to the clouding of the back part of the natural lens before surgery. Though these conditions share similarities, their symptoms differ in subtle ways:
Symptom | Posterior Cataract | Secondary Cataract (PCO) |
Blurred Vision | Gradual loss of clarity due to lens opacification. | Blurred or hazy vision from capsule clouding. |
Glare and Halos | Pronounced glare in bright lights, often at night. | Similar glare and halos, especially noticeable post-surgery. |
Contrast Sensitivity | Decreased due to natural lens opacity. | Reduced due to capsule thickening. |
Onset Timing | Develops gradually before surgery. | Appears weeks, months, or years after surgery. |
Progression | Progresses slowly over time without treatment. | Can worsen steadily without treatment. |
While both conditions impair vision, PCO arises post-surgery and is treatable with a YAG laser capsulotomy, whereas posterior cataracts require surgical lens replacement.
What are the risk factors for a secondary cataract?
Certain factors can increase the likelihood of developing a secondary cataract after cataract surgery:
Age:
Younger patients have a higher risk due to more active lens epithelial cells.
Surgical Technique:
Less precise removal of lens material during cataract surgery can leave behind more residual epithelial cells, raising the risk.
Type of Intraocular Lens (IOL):
Older IOL designs or those without sharp edges are associated with a higher risk of posterior capsule opacification.
Preexisting Conditions:
Eye disorders such as uveitis (inflammation of the eye), diabetes, or glaucoma can increase susceptibility.
Trauma or Complications During Surgery:
Surgical challenges or complications may promote cell migration, leading to opacification.
Genetic Predisposition:
Individual healing responses and genetic factors may influence the risk of capsule clouding.
By understanding these risk factors, patients and surgeons can take preventive measures to minimize the likelihood of developing this condition.
How is posterior capsular opacification diagnosed?
Diagnosis of posterior capsular opacification typically involves a comprehensive eye examination conducted by an ophthalmologist. Key steps in the diagnostic process include:
Patient History: The doctor asks about symptoms such as blurry vision, glare, or difficulty with daily activities. They may also review the patient’s cataract surgery history.
Visual Acuity Test: This test assesses the sharpness of vision to identify any loss or deterioration.
Slit-Lamp Examination: A detailed inspection of the eye using a specialized microscope helps identify the clouding of the posterior capsule.
Pupil Dilation: The eye is dilated with medicated drops to allow a better view of the posterior segment and confirm the diagnosis.
Differential Diagnosis: The ophthalmologist rules out other potential causes of vision problems, such as retinal detachment or macular degeneration.
These steps ensure an accurate diagnosis and guide the treatment plan.
What treatment options are available for posterior capsular opacification?
The primary treatment for posterior capsular opacification is a non-invasive outpatient procedure called a YAG laser capsulotomy. Here’s how it works:
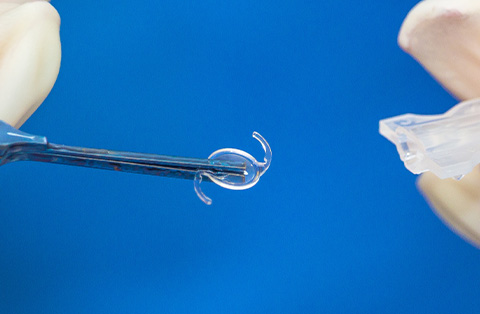
YAG Laser Capsulotomy:
A laser creates a small opening in the cloudy posterior capsule.
This allows light to pass through unobstructed, restoring clear vision.
The procedure is quick, usually taking only a few minutes, and does not require an incision.
Benefits:
Immediate improvement in vision for most patients.
No significant recovery time—normal activities can usually be resumed the same day.
Alternative Management:
In rare cases where laser treatment isn’t suitable, other options may include surgical removal of the opacified capsule, though this is uncommon.
Timely treatment can prevent long-term complications and significantly improve quality of life.
YAG Laser Capsulotomy
YAG laser capsulotomy is the standard treatment for posterior capsular opacification. It is a quick, safe, and effective outpatient procedure that restores vision by removing the clouded area of the posterior capsule.
Step-by-Step Process:
Preparation:
The doctor applies anesthetic eye drops to prevent discomfort.
Pupil-dilating drops are used to provide a better view of the posterior capsule.
Procedure:
The patient sits at a laser machine, similar to a slit-lamp examination.
The YAG laser focuses on the clouded capsule and creates a small, precise opening in its center.
This allows light to pass through the lens implant and reach the retina, restoring clear vision.
Duration:
The procedure typically takes 5–10 minutes.
Post-Treatment:
Vision improvement is often noticeable within hours.
The doctor may prescribe anti-inflammatory eye drops to prevent swelling or irritation.
Benefits of YAG Laser Capsulotomy:
Non-invasive: No incisions or surgical tools are involved.
Quick Recovery: Most patients return to their normal activities the same day.
Effective: Provides lasting relief from symptoms with minimal risks.
Potential Risks (Rare):
Temporary floaters in vision.
Slight increase in eye pressure, which is usually monitored and managed.
Rarely, retinal detachment or macular edema.
YAG laser capsulotomy is a widely used and reliable procedure, with most patients experiencing significant improvement in their vision.
How soon after YAG laser capsulotomy treatment will I feel better?
Most patients experience improvement in their vision very quickly after the procedure.
Immediate Effects:
Vision may start to clear within a few hours of treatment.
Some patients notice sharper vision immediately after the procedure.
Short-Term Symptoms:
Temporary floaters may appear due to tiny debris created during the laser treatment. These usually fade within a few days to weeks.
Mild sensitivity to light may occur but resolves quickly.
Full Recovery:
Most individuals achieve optimal visual clarity within 24–48 hours.
Normal daily activities can typically be resumed the same day or the next.
The rapid recovery and significant improvement in vision make YAG laser capsulotomy a highly effective treatment for posterior capsular opacification.
Can posterior capsular opacification go away by itself?
Posterior capsular opacification does not resolve on its own. Once the posterior capsule becomes cloudy, the symptoms typically persist and may gradually worsen over time. The underlying cause is the growth and thickening of residual lens epithelial cells on the capsule.
Without treatment, PCO continues to impair vision, affecting daily activities like reading, driving, and recognizing faces. A YAG laser capsulotomy is the only effective way to clear the opacification and restore vision. This procedure is quick, safe, and provides lasting relief.
Can posterior capsular opacification be prevented?
While posterior capsular opacification cannot always be fully prevented, certain steps during and after cataract surgery can reduce its likelihood:
During Cataract Surgery:
Advanced Intraocular Lens (IOL) Design:
Modern lenses with special edge designs, such as square-edged IOLs, reduce cell migration that causes capsule clouding.
Thorough Lens Material Removal:
Surgeons carefully remove as much residual lens material as possible to minimize the risk of opacification.
After Surgery:
Regular Follow-Ups: Early detection of capsule thickening during routine eye exams allows for timely management before symptoms worsen.
Although these measures help, PCO remains a common complication due to the body’s natural healing response. For those who develop it, a YAG laser capsulotomy effectively resolves the issue.