What is Mandibular Osteotomy?
Mandibular osteotomy is a surgical procedure targeting the lower jaw (mandible). Surgeons cut and reposition the mandible to correct misalignments such as underbites, overbites, or asymmetry. This surgery aims to improve jaw function and facial aesthetics, enhancing both the patient's bite and appearance.
Key Differences Between Mandibular Osteotomy and Other Jaw Surgeries
Mandibular osteotomy focuses on the lower jaw, correcting its alignment for improved function and aesthetics. Unlike maxillary osteotomy, which adjusts the upper jaw, or orthognathic surgeries like LeFort that reposition the midface, mandibular osteotomy specifically targets mandibular issues. It directly addresses underbites, overbites, and jaw asymmetry exclusive to the lower jaw.
Surgery Type | Jaw Targeted | Primary Correction Focus |
Mandibular Osteotomy | Lower Jaw (Mandible) | Underbites, Overbites, Asymmetry |
Maxillary Osteotomy | Upper Jaw (Maxilla) | Overbites, Underbites, Crossbites |
LeFort I, II, III | Midface to Upper Jaw | Vertical and Horizontal Maxilla Adjustments |
The Role of the Maxillofacial Surgeon in Mandibular Osteotomy
The maxillofacial surgeon plays a critical role in mandibular osteotomy. They assess the jaw's misalignment, plan the surgical approach, and perform the operation. Their expertise ensures the jaw moves to the correct position, improving bite and appearance. Post-surgery, they guide recovery, overseeing wound care and jaw function restoration. Their skill and knowledge in oral and maxillofacial surgery are crucial for successful outcomes.
Preparing for Your Lower Jaw Surgery: Steps and Considerations
Preparing for your lower jaw surgery involves several crucial steps. First, undergo detailed consultations with your maxillofacial surgeon to understand the procedure and outcomes. Next, complete necessary dental treatments. Then, get imaging tests like X-rays for precise planning. Finally, follow pre-surgery instructions, including fasting and medication adjustments. Proper preparation ensures a smoother procedure and recovery.
Consultation: Discuss the procedure, risks, and expected outcomes with your surgeon.
Dental Work: Address any dental issues to ensure optimal surgery results.
Imaging Tests: X-rays and scans help in planning the surgery with accuracy.
Pre-surgery Instructions: Includes fasting and managing medications, preparing your body for surgery.
What to Expect During the Mandibular Osteotomy Procedure
During the mandibular osteotomy procedure, expect general anesthesia for comfort. The surgeon makes cuts inside the mouth to access the lower jaw, minimizing visible scars. They then carefully cut the jawbone, repositioning it for optimal alignment. The jaw is secured with screws and plates. The procedure typically lasts several hours, focusing on precise adjustments for improved jaw function and appearance.
Pre-Surgical Assessments and Orthodontic Requirements
Pre-surgical assessments for mandibular osteotomy involve detailed imaging, like X-rays and 3D scans, to visualize the jaw's structure. Orthodontic requirements usually include braces to align teeth pre-surgery, ensuring they fit correctly post-procedure. These steps are crucial for planning a successful surgery, customizing the approach to each patient's needs, and optimizing outcomes for function and aesthetics.
The Surgical Process: Inside the Operation Room
In the operation room, the surgical team prepares the patient under general anesthesia. The maxillofacial surgeon makes precise incisions inside the mouth to access the lower jaw. They then cut the bone, carefully repositioning the mandible. Special plates and screws secure the new position. Throughout, the team monitors vital signs, ensuring the patient's safety and the surgery's success.
Techniques and Tools: Incision, Screw, and Plate Placement
Surgeons use specific techniques and tools for mandibular osteotomy. They make incisions inside the mouth to avoid visible scars. The team then uses specialized tools to cut the jawbone precisely. They reposition the mandible and secure it with screws and plates, ensuring stability. These titanium fixtures support bone healing in the new alignment, crucial for the jaw's function and appearance.
Understanding the Risks and Complications of Jaw Surgery
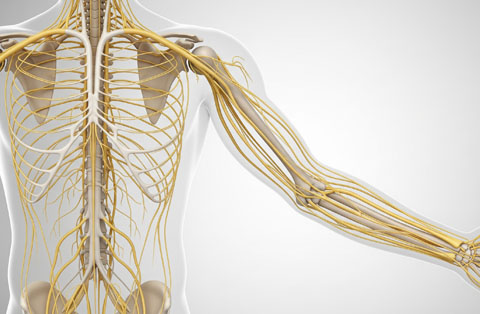
Understanding the risks and complications of jaw surgery is important. These can include infection, nerve damage leading to numbness, and issues with jaw alignment. Bleeding and reaction to anesthesia are also potential risks. Proper planning and post-operative care reduce these risks significantly. Discussing these concerns with your surgeon before the procedure can help manage expectations and prepare for recovery.
Advancements in Mandibular Osteotomy Techniques
Advancements in mandibular osteotomy techniques have significantly improved outcomes and recovery times.
Surgeons now use 3D imaging for precise planning, customizing each procedure to the patient's specific anatomy. Computer-assisted surgery enhances accuracy, allowing for more predictable results.
The development of biocompatible screws and plates has also improved bone healing and stability. Minimally invasive approaches reduce trauma, leading to less post-operative pain and quicker recovery. These innovations not only ensure the surgery's success but also enhance patient comfort and satisfaction, marking a new era in the field of maxillofacial surgery.
Recovery and Post-Operative Care: What to Expect
Expect swelling and discomfort in the initial recovery phase after mandibular osteotomy. Pain management and a liquid or soft diet are essential. Follow your surgeon's instructions closely for oral hygiene to prevent infection. Gradually, you'll return to normal activities, with follow-up visits to monitor healing. Adhering to post-operative care guidelines ensures a smooth recovery and successful surgical outcome.
The First Few Days Following Surgery: Managing Pain and Swelling
In the first few days following surgery, managing pain and swelling is crucial. Use prescribed pain medication as directed. Apply ice packs to reduce swelling. Keep your head elevated, even while sleeping, to help decrease swelling faster. Eat soft foods and stay hydrated. Follow all post-surgical care instructions your surgeon provides to minimize discomfort and ensure a smooth initial recovery period.
Long-Term Recovery: Diet, Exercise, and Follow-up Visits
Long-term recovery involves careful attention to diet, exercise, and follow-up visits. Gradually reintroduce solid foods as healing progresses. Incorporate gentle exercises once your surgeon approves, avoiding strenuous activities. Attend all follow-up visits to monitor your recovery and adjust any necessary treatments. Consistently following these guidelines supports effective healing, ensuring the best possible outcome from your mandibular osteotomy.
Life After Mandibular Osteotomy: Adjusting to the New Position of Your Lower Jaw
Life after mandibular osteotomy involves adjusting to the new position of your lower jaw. Initially, you may notice changes in biting and chewing, which gradually improve. Speech may also temporarily alter but will normalize as you adapt. Follow-up orthodontic treatment often refines alignment. Embrace the positive changes in appearance and function, enhancing self-confidence and overall quality of life.
Comparing Mandibular Advancement vs. Setback: What's Best for You?
Comparing mandibular advancement to setback depends on your specific jaw issues. Advancement moves the jaw forward, ideal for correcting underbites. Setback shifts the jaw back, suited for overbites. The best choice aligns with your dental needs, facial symmetry, and desired outcomes. A thorough consultation with a maxillofacial surgeon determines which procedure optimally addresses your condition, ensuring the best aesthetic and functional results.
Assessing the Need for Advancement or Setback in Lower Jaw Surgery
Assessing the need for advancement or setback in lower jaw surgery involves examining your jaw's alignment and bite issues. Advancement corrects underbites by moving the jaw forward, while setback addresses overbites by repositioning it backward. A detailed evaluation by a maxillofacial surgeon, including imaging studies, determines the appropriate approach to achieve optimal balance, function, and aesthetics for your specific condition.
The Impact of Mandibular Position on Facial Aesthetics and Functionality
The mandibular position significantly impacts facial aesthetics and functionality. Proper alignment ensures a balanced appearance and harmonious facial proportions. It also improves bite function, making eating and speaking more efficient. Misalignments can cause aesthetic concerns and functional problems. Correcting these with mandibular osteotomy enhances both the look and effectiveness of facial structures, boosting confidence and quality of life.
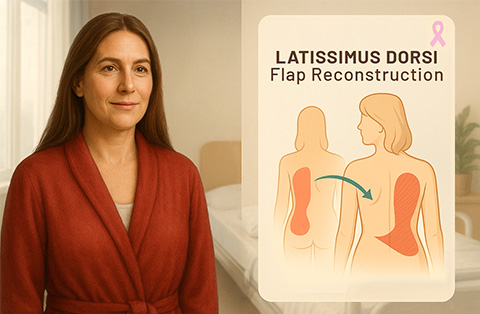
Other Procedures Related to Mandibular Osteotomy
Other procedures related to mandibular osteotomy include genioplasty, which reshapes the chin, and maxillary osteotomy for the upper jaw. Orthodontic treatments, like braces, often accompany these surgeries to align teeth properly.
Temporomandibular joint (TMJ) therapies may also follow to ensure joint health. These complementary procedures enhance overall facial symmetry and function, offering a comprehensive approach to correcting jaw and dental issues.
Maxillary Osteotomy: Correcting the Upper Jaw in Conjunction with Lower Jaw Surgery
Maxillary osteotomy corrects the upper jaw in conjunction with lower jaw surgery to achieve comprehensive facial and bite alignment. This approach ensures the jaws work together harmoniously, improving overall aesthetics and function. It addresses issues like severe overbites or underbites, creating a balanced facial profile and efficient chewing mechanics. This coordinated effort results in optimal outcomes for both appearance and oral health.
Genioplasty: Fine-Tuning the Chin Post-Mandibular Osteotomy
Genioplasty fine-tunes the chin's appearance after mandibular osteotomy. This surgical procedure adjusts the chin's size and shape, enhancing facial harmony. It complements the jaw's new position, ensuring the lower facial profile is balanced. Genioplasty can either advance or reduce the chin, tailored to each patient's needs, contributing to improved aesthetics and confidence.
Bimaxillary Osteotomy: When Both Upper and Lower Jaws Require Surgery
Bimaxillary osteotomy involves surgery on both the upper and lower jaws. This approach corrects significant skeletal discrepancies, aligning the jaws properly. It addresses severe bite issues, facial asymmetry, and aesthetic concerns in a comprehensive manner. Performing surgery on both jaws ensures optimal function and facial harmony, providing a balanced and aesthetically pleasing outcome.
Maxillofacial Surgeon for Orthognathic Surgery
A maxillofacial surgeon specializes in orthognathic surgery, correcting jaw and facial bone structures. They assess patients' needs, plan precise surgical interventions, and perform complex procedures to improve facial symmetry and function. Their expertise ensures successful outcomes, enhancing patients' quality of life through improved aesthetics and jaw functionality.
Risks and Complications
Mandibular osteotomy carries risks and complications like any surgical procedure. Patients may experience nerve damage, leading to numbness. Infection and bleeding are possible. Improper healing can result in misalignment or the need for additional surgery. Discussing these risks with your surgeon is important for informed decision-making.
Nerve damage
Infection
Bleeding
Misalignment
Need for further surgery
Frequently Asked Questions
What is the recovery time for a mandibular osteotomy?
The recovery time for a mandibular osteotomy typically ranges from 6 to 12 weeks for initial healing. Full recovery, including complete bone healing and orthodontic adjustments, can take up to a year. Patients gradually return to normal activities, following their surgeon's guidance for a smooth recovery.
Is mandibular osteotomy painful?
Mandibular osteotomy involves some pain and discomfort, especially in the days following the surgery. However, pain management techniques and medications effectively reduce these symptoms. Most patients find the discomfort manageable and notice significant improvement within the first few weeks as they heal.
What is the age limit for jaw surgery?
There is no strict age limit for jaw surgery. However, surgeons typically recommend waiting until after growth stops, usually around 16-18 years for females and 18-21 years for males. Adults of any age can undergo surgery, provided they are in good overall health.
Can you talk after jaw surgery?
After jaw surgery, patients can talk, but they might find it challenging initially. Surgeons often advise minimal talking to avoid strain on the jaw. As swelling decreases and healing progresses, speech becomes easier. Full return to normal speaking ability varies with individual recovery rates.
How much is jaw surgery in Turkey?
The cost of jaw surgery in Turkey varies widely based on the complexity of the procedure and the clinic's reputation. On average, prices range from $3,000 to $7,000. This cost is generally lower compared to many Western countries, making Turkey a popular destination for medical tourism.
Does jaw surgery affect brain?
Jaw surgery does not affect the brain. The procedures are localized to the jaw and facial structure, ensuring no impact on brain function. Surgeons take great care to operate precisely within the targeted area, maintaining the safety and integrity of surrounding tissues and organs.