Struggling with sleep apnea and loud snoring? Tongue base surgery can open your airway, reduce apnea episodes, and improve sleep quality. Breathe better, sleep deeper, and wake up refreshed.
What is tongue base surgery?
Tongue base surgery is a procedure to reduce the size of the tongue base, which can block the airway during sleep. It is often used to treat obstructive sleep apnea (OSA) in patients with an enlarged tongue base. The surgery helps improve airflow by removing or repositioning excess tissue.
Different techniques include radiofrequency ablation, coblation, midline glossectomy, and robotic-assisted surgery. The choice of procedure depends on the severity of the obstruction and the patient’s condition.
What is obstructive sleep apnea syndrome?
Obstructive sleep apnea syndrome (OSAS) is a sleep disorder where the airway repeatedly becomes blocked during sleep, causing breathing to stop and start. This happens when the throat muscles relax too much, allowing the tongue or soft tissues to collapse and obstruct airflow.
Key Characteristics
Repeated Breathing Pauses: Episodes last from a few seconds to over a minute and occur multiple times per hour.
Oxygen Level Drops: Reduced airflow lowers blood oxygen, forcing the brain to wake the body.
Disrupted Sleep: Frequent awakenings prevent deep, restorative sleep.
Common Symptoms
Loud snoring
Gasping or choking during sleep
Excessive daytime sleepiness
Morning headaches
Difficulty concentrating
Irritability and mood changes
If untreated, OSAS increases the risk of high blood pressure, heart disease, stroke, and diabetes. Treatments include lifestyle changes, CPAP therapy, oral appliances, and surgery for severe cases.
How does it help with obstructive sleep apnea?
Tongue base surgery helps treat obstructive sleep apnea (OSA) by reducing airway blockage caused by an enlarged tongue base. During sleep, the tongue can collapse backward, obstructing airflow and causing breathing pauses. This surgery removes or reshapes excess tissue, creating a larger airway space.
Understanding the tongue base and its role in sleep
The tongue base is the lower part of the tongue, located near the throat. It plays a crucial role in breathing, swallowing, and speaking. During sleep, muscle tone in the tongue relaxes. In some individuals, especially those with a large tongue base or weak muscle tone, the tongue can collapse backward and block the airway.
This obstruction reduces airflow, leading to snoring and breathing pauses, which are key signs of obstructive sleep apnea (OSA). When the airway is blocked, oxygen levels drop, forcing the brain to wake the body to restore breathing. This cycle disrupts sleep quality and can lead to serious health issues if untreated.
How surgery for sleep apnea targets the back of the tongue?
Surgery for sleep apnea targets the back of the tongue by reducing its size or repositioning it to prevent airway obstruction. The goal is to create more space in the throat, allowing better airflow during sleep.
Techniques used include:
Radiofrequency Ablation (RFA): Uses heat energy to shrink tongue tissue over time.
Coblation Surgery: Removes excess tissue with controlled plasma technology.
Midline Glossectomy: Surgically removes a portion of the tongue base.
Robotic-Assisted Surgery: Provides precise tissue removal with minimal damage.
Hyoid Suspension: Repositions structures around the tongue for better airway support.
These procedures help reduce apnea episodes and improve sleep quality.
The benefits of tongue reduction in sleep apnea treatment
Tongue reduction surgery helps improve airflow and reduce airway obstruction in sleep apnea patients. By shrinking or repositioning the tongue base, the procedure enhances breathing during sleep.
Key benefits include:
Fewer apnea episodes – Reduces airway blockages that cause breathing pauses.
Better oxygen levels – Improves oxygen intake, lowering health risks.
Reduced snoring – Decreases vibrations in the airway for quieter sleep.
Improved sleep quality – Leads to deeper, more restful sleep.
Less reliance on CPAP – Helps patients who struggle with CPAP therapy.
For the best results, tongue surgery is often combined with other airway procedures.
Is it effective on snoring?
Yes, tongue base surgery is effective in reducing snoring, especially in patients with obstructive sleep apnea (OSA). Snoring occurs when airway tissues vibrate due to partial obstruction. If the tongue base is a primary cause of the blockage, surgery can significantly decrease snoring.
How It Helps Reduce Snoring?
Removes Excess Tissue: Reduces the bulk of the tongue base, preventing airway narrowing.
Improves Airflow: Creates a larger airway space, reducing turbulence that causes snoring.
Stabilizes the Tongue: Prevents it from collapsing backward during sleep.
While many patients experience noticeable snoring reduction, results vary. Some may need additional treatments, such as soft palate surgery or lifestyle changes, for the best outcome.
How is surgery for sleep apnea performed?
Tongue base surgery for sleep apnea is performed under general anesthesia in a hospital or surgical center. The specific technique used depends on the severity of airway obstruction and the patient's anatomy. The goal is to reduce the size of the tongue base or reposition it to prevent airway collapse during sleep.
Preoperative Preparation
Before surgery, the patient undergoes a thorough evaluation, including:
A sleep study (polysomnography) to assess the severity of sleep apnea.
Imaging tests (MRI or CT scans) to evaluate airway obstruction.
An airway examination using a flexible endoscope.
A review of medical history and any previous sleep apnea treatments.
Surgical Techniques
Several procedures can target the tongue base, either alone or in combination with other airway surgeries.
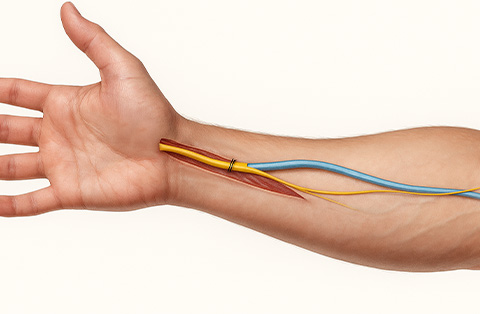
Radiofrequency Ablation (RFA)
A minimally invasive procedure performed under local or general anesthesia.
A thin probe is inserted into the tongue base, delivering controlled radiofrequency energy.
This heat shrinks and stiffens the tissue over time, reducing its tendency to collapse.
Multiple sessions (usually 3–5) may be needed for optimal results.
Coblation Tongue Reduction
Uses controlled plasma energy to remove excess tissue while minimizing bleeding and damage to surrounding structures.
The surgeon inserts a wand-like device into the tongue base through the mouth.
The device generates plasma energy that dissolves soft tissue at low temperatures.
Healing occurs over several weeks, with gradual improvement in airflow.
Midline Glossectomy and Lingualplasty
Involves surgically removing a portion of the tongue base to create more space in the airway.
Performed through the mouth using specialized instruments.
The surgeon carefully excises tissue from the middle of the tongue base.
In some cases, lingualplasty is done to reshape the tongue for better airway support.
Robotic-Assisted Transoral Surgery (TORS)
A highly precise, minimally invasive procedure using robotic arms and a 3D camera.
The surgeon operates through the mouth, controlling robotic instruments to remove excess tissue.
Offers better visibility and accuracy compared to traditional surgery.
Results in less pain, faster recovery, and improved breathing.
Hyoid Suspension (If Needed)
The hyoid bone (a small U-shaped bone in the neck) is repositioned to help stabilize the tongue and airway.
This procedure is often combined with tongue reduction for better results.
Postoperative Care and Recovery
Patients typically stay in the hospital for monitoring, especially if they have severe sleep apnea.
Swelling and throat discomfort are common and managed with pain medication.
A soft or liquid diet is recommended for the first few days.
Full recovery can take several weeks, with gradual improvement in breathing and sleep quality.
Results vary based on the severity of sleep apnea and the specific procedure performed. Many patients experience fewer apnea episodes, better oxygen levels, and improved sleep.
What are the potential risks and complications of tongue base surgery?
Tongue base surgery is generally safe, but like any surgical procedure, it carries some risks. The complexity of the surgery depends on the technique used and the patient’s anatomy. Most complications are temporary and manageable.
Possible Risks and Complications
Swelling and Airway Obstruction: Temporary swelling may narrow the airway, causing breathing difficulty in the first few days.
Pain and Discomfort: Sore throat, tongue pain, and difficulty swallowing are common during recovery.
Bleeding: Mild bleeding is expected, but severe bleeding is rare and may require intervention.
Infection: Though uncommon, infections can occur and may need antibiotics.
Speech and Swallowing Changes: Some patients experience temporary speech changes or difficulty swallowing.
Numbness or Altered Sensation: Nerve irritation can cause temporary numbness in the tongue or throat.
Scarring and Stiffness: Healing may lead to minor scarring, which can affect tongue movement.
Need for Additional Treatment: Some patients may require multiple procedures or combination therapies for the best results.
Most side effects improve within a few weeks, and serious complications are rare when performed by an experienced surgeon.
How effective is tongue base suspension with uvulopalato-pharyngoplasty on sleep quality?
Tongue base suspension combined with uvulopalatopharyngoplasty (UPPP) is an effective treatment for obstructive sleep apnea (OSA) in selected patients. UPPP removes excess tissue from the soft palate and throat, while tongue base suspension stabilizes the tongue to prevent airway collapse. Together, these procedures improve airflow and reduce apnea episodes.
Effectiveness on Sleep Quality
Reduced Apnea-Hypopnea Index (AHI): Studies show significant reductions in the number of breathing pauses per hour.
Improved Oxygen Levels: Better airflow leads to higher blood oxygen levels during sleep.
Decreased Snoring: Removing excess tissue and stabilizing the tongue help reduce snoring intensity.
Better Sleep Continuity: Fewer breathing interruptions lead to deeper, more restful sleep.
Less CPAP Dependence: Some patients experience reduced reliance on CPAP therapy.
Success rates vary based on the severity of OSA and patient anatomy. The combination procedure is most effective in patients with multi-level airway obstruction.