Restore clear vision and regain daily comfort with phacoemulsification: the modern, safe, and effective solution for cataracts using advanced ultrasound technology and intraocular lenses.
What is Phacoemulsification in Modern Cataract Surgery?
Phacoemulsification is a modern technique used in cataract surgery. It involves the removal of the eye's natural lens when it becomes cloudy due to cataract formation. This method uses ultrasonic vibrations to break the cloudy lens into tiny fragments. The surgeon then gently suctions out these fragments through a small incision.
This technique allows for a minimally invasive procedure. It preserves most of the eye's natural structures. After the cloudy lens is removed, a clear artificial intraocular lens (IOL) is implanted in its place. Phacoemulsification is the most commonly used method in cataract surgery today due to its safety, precision, and quick recovery time.
How does phacoemulsification work?
Phacoemulsification works through a series of precise steps. It uses a combination of ultrasound energy, micro-incisions, and advanced surgical tools. The goal is to remove the cloudy lens safely and replace it with a clear artificial lens.
Here is how the procedure works in detail:
1. Local anesthesia:
The surgeon numbs the eye using eye drops or a small injection. The patient remains awake but feels no pain.
2. Small incision:
A small incision, usually around 2 to 3 millimeters, is made at the edge of the cornea. This allows access to the lens without the need for stitches.
3. Capsulorhexis:
The surgeon creates a circular opening in the thin capsule that surrounds the lens. This gives access to the cloudy lens inside.
4. Ultrasound probe insertion:
A special probe that emits ultrasonic vibrations is inserted through the incision. The probe breaks the cloudy lens into tiny fragments. This process is called emulsification.
5. Suction of lens fragments:
The same probe or a separate instrument suctions out the broken lens pieces from the eye.
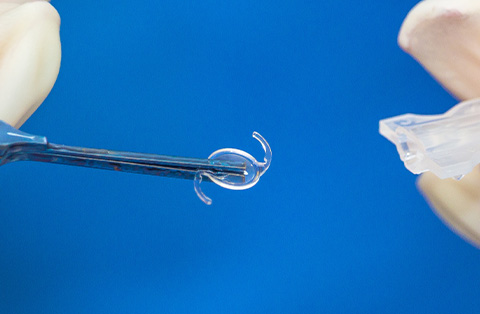
6. Intraocular lens (IOL) implantation:
After all fragments are removed, the surgeon implants a folded artificial intraocular lens through the same small incision. The lens unfolds inside the eye and is positioned securely in the lens capsule.
7. Final adjustments:
The surgeon checks the position of the lens and ensures the eye is stable. In most cases, the incision is self-sealing and does not need stitches.
This method reduces surgical trauma and shortens recovery time. It also lowers the risk of complications compared to older techniques.
Advantages of using phacoemulsification over traditional methods
Phacoemulsification offers several advantages over traditional cataract surgery methods, such as extracapsular cataract extraction (ECCE). These benefits have made it the preferred technique in modern ophthalmology.
Smaller incision: Phacoemulsification uses a 2 to 3 mm incision, while traditional methods require a much larger cut. A smaller incision leads to faster healing, less discomfort, and a reduced risk of infection.
No need for stitches: In most cases, the incision is self-sealing. This means no sutures are required. This shortens surgery time and improves postoperative comfort.
Faster visual recovery: Patients regain clear vision more quickly. Most can resume normal activities within a few days.
Less trauma to the eye: The ultrasonic probe breaks the lens into tiny fragments without removing the lens in one piece. This results in less stress to the eye and surrounding tissues.
Better surgical control: The surgeon can work with greater precision using modern phacoemulsification machines. This improves outcomes and lowers complication rates.
Improved refractive results: The use of advanced intraocular lenses and accurate measurements helps correct pre-existing vision problems, such as nearsightedness or astigmatism.
These advantages make phacoemulsification a safer and more effective choice for most patients undergoing cataract surgery.
The role of the phaco tip and foot pedal in the process
The phaco tip and foot pedal are two essential components in the phacoemulsification system. They work together to ensure the controlled and safe removal of the cataract.
Phaco tip:
The phaco tip is a thin, hollow metal probe that delivers ultrasonic energy. It is inserted into the eye through the small corneal incision. The tip vibrates at high frequency, breaking the cloudy lens into microscopic fragments. It also creates a vacuum to aspirate these fragments from the eye.
Modern phaco tips are designed to reduce heat and damage to surrounding tissues. Some have specialized shapes to improve cutting efficiency and fluid control.
Foot pedal:
The surgeon uses the foot pedal to control the phaco machine. It has multiple levels of pressure that activate different functions:
The first level controls irrigation to maintain the shape of the eye
The second level activates aspiration to remove lens fragments
The third level delivers ultrasonic power to emulsify the lens
The foot pedal allows the surgeon to switch between these functions without taking their hands off the instruments. This ensures precise control and smooth operation throughout the procedure.
Together, the phaco tip and foot pedal provide the tools needed for safe and effective cataract removal.
How Does Cataract Surgery with Intraocular Lens Work?
Cataract surgery with an intraocular lens (IOL) involves removing the eye’s cloudy natural lens and replacing it with a clear artificial lens. This restores vision affected by cataracts. The procedure is typically performed using phacoemulsification.
Steps involved in cataract surgery
Here is how the process works:
Cataract removal: The surgeon uses phacoemulsification to break and remove the cloudy lens. This is done through a small incision with minimal impact on surrounding tissues.
IOL selection: Before surgery, the eye is measured to choose the right intraocular lens. The type and power of the lens depend on the patient’s vision needs. Options include monofocal, multifocal, or toric lenses.
IOL implantation: After removing the cataract, the surgeon inserts the folded IOL through the same small incision. Once inside the eye, the lens unfolds and is positioned in the lens capsule.
Lens positioning: The surgeon ensures the IOL is centered and stable. It remains in place permanently and does not require maintenance.
The IOL functions like a natural lens. It focuses light onto the retina, allowing the patient to see clearly again. Most patients experience significant improvement in vision shortly after surgery.
Importance of intraocular lens in restoring vision
The intraocular lens (IOL) plays a critical role in restoring vision after cataract surgery. When the natural lens becomes cloudy due to a cataract, it blocks and scatters light. This reduces visual clarity and causes symptoms like blurred vision and glare. Removing the cataract without replacing the lens would leave the eye without a focusing structure.
The IOL replaces the removed natural lens and restores the eye’s ability to focus light onto the retina. This allows the patient to see clearly again.
Key functions of the intraocular lens:
Light refraction: The IOL bends incoming light and directs it to the retina, enabling clear vision.
Permanent solution: Once implanted, the IOL remains stable and functional for life. It does not need replacement or maintenance.
Custom vision correction: IOLs can be selected to correct nearsightedness, farsightedness, astigmatism, or presbyopia. This reduces or eliminates the need for glasses.
High biocompatibility: Modern IOLs are made from materials like acrylic or silicone. These are well-tolerated by the eye and rarely cause reactions.
The IOL is essential for achieving good visual outcomes in cataract surgery. It not only restores lost vision but can also improve overall visual quality.
How surgeons choose the right intraocular lens?
Surgeons choose the right intraocular lens (IOL) based on several factors specific to each patient. The goal is to restore clear vision and meet individual visual needs after cataract surgery.
Key factors in IOL selection:
Eye measurements:
The surgeon measures the eye’s length and corneal curvature using advanced imaging tools. These values help calculate the exact IOL power needed.Vision goals:
The patient’s lifestyle and visual preferences are considered. Some patients want clear distance vision, while others prefer less dependence on glasses for reading or intermediate tasks.Pre-existing conditions:
Conditions like astigmatism, macular degeneration, or prior eye surgery can influence IOL choice. For example, toric lenses are used for patients with significant astigmatism.Type of IOL:
Surgeons choose among monofocal, multifocal, extended depth of focus (EDOF), or toric lenses. Each type offers different benefits and limitations.Pupil size and eye health:
Factors like pupil function and the health of the retina and cornea can affect how well certain lenses perform.
By carefully evaluating these aspects, surgeons aim to select the IOL that provides the best possible visual outcome for each patient.
What Are the Risks and Complications in Phacoemulsification Surgery?
Phacoemulsification is a common and generally safe procedure. Most patients recover with improved vision and no serious issues. However, like all surgeries, it carries some risks.
Possible risks and complications include:
Infection (endophthalmitis): Rare but serious. Can lead to vision loss if not treated quickly.
Posterior capsule opacification (PCO): A common long-term issue. The capsule holding the IOL becomes cloudy. Treatable with a quick laser procedure.
Inflammation: Mild swelling or redness may occur. Usually controlled with eye drops.
Retinal detachment: Rare. Higher risk in patients with high myopia or prior eye trauma.
Intraocular pressure rise: Temporary increase in eye pressure. Typically resolves with medication.
Dislocated intraocular lens: The lens may shift from its position. May require surgical repositioning.
Corneal swelling or damage: Can affect vision. Usually temporary but may need treatment.
Bleeding inside the eye: Rare. Managed by close monitoring or additional surgery if needed.
Phacoemulsification is considered a low-risk procedure when performed by an experienced surgeon. Most complications can be managed effectively if detected early.
Who Are the Ideal Candidates for Phacoemulsification?
Ideal candidates for phacoemulsification are patients with cataracts that affect their daily vision and quality of life. The procedure is suitable for most individuals with age-related or early-stage cataracts.
Common traits of ideal candidates include:
Stable general health: Patients should be healthy enough to undergo local anesthesia and outpatient surgery.
Visually significant cataract: Cataracts must cause noticeable vision problems, such as blurred vision, glare, or difficulty reading and driving.
Healthy cornea and retina: A clear cornea and good retinal function are essential for optimal surgical outcomes.
Normal eye pressure: Patients should not have uncontrolled glaucoma or other conditions that affect intraocular pressure.
No active eye infections or inflammation: The eye must be free from any current infection or uveitis.
Realistic expectations: Candidates should understand the potential outcomes and limitations of surgery, including the need for glasses depending on the IOL type.
Phacoemulsification is also preferred for patients who want faster recovery, smaller incisions, and minimal postoperative discomfort.