Nerve injury occurs when a nerve is damaged by trauma, compression, or disease, disrupting the signals between the brain, spinal cord, and body.
These injuries matter because they can cause weakness, numbness, or pain, and in severe cases, permanent loss of function. Early diagnosis and treatment improve recovery, yet many cases go unrecognized until damage is advanced.
In this guide, we explain what nerves are, causes and symptoms of nerve injuries, how they’re diagnosed, treatment options, including surgical techniques, and what to expect during recovery.
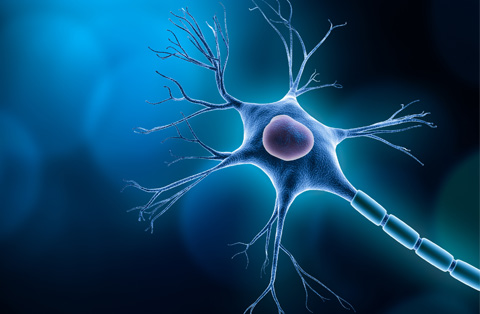
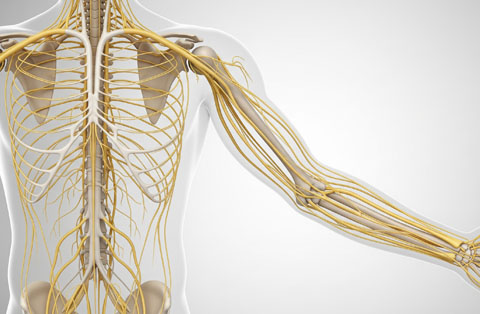
What is a nerve?
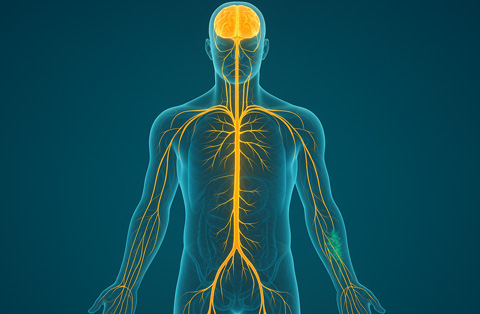
A nerve is a bundle of fibers that carries messages between the brain, spinal cord, and the rest of the body. These messages control movement, sensation, and many involuntary functions such as breathing and digestion.
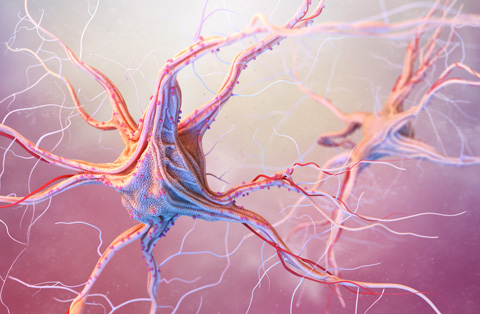
Nerves are made up of specialized cells called neurons. Each neuron has long projections, known as axons, that transmit electrical signals. Surrounding tissues, including connective tissue layers and a protective myelin sheath, insulate and support these signals.
The body has three main types of nerves:
Sensory nerves transmit information from the skin, muscles, and organs to the brain.
Motor nerves send signals from the brain and spinal cord to muscles, controlling movement.
Autonomic nerves manage automatic functions such as heart rate, blood pressure, and digestion.
Healthy nerves ensure that messages travel quickly and accurately. When a nerve is injured, these signals can be disrupted, leading to symptoms such as weakness, numbness, or pain.
What causes a nerve injury?
A nerve injury happens when physical force, pressure, or disease disrupts the structure or function of a nerve. This damage can block or distort the electrical signals that nerves use to carry messages.
The main causes include:
Direct trauma: Cuts, crush injuries, or blunt force can sever or compress nerves.
Pressure: Prolonged compression from bone fractures, tight casts, or repetitive motion can injure nerves.
Stretching: Sudden or excessive movement of a limb can overstretch and damage nerve fibers.
Medical conditions: Diabetes, autoimmune diseases, infections, and certain cancers can damage nerves over time.
Toxic exposure: Alcohol abuse, certain medications, or heavy metals can impair nerve health.
In many cases, a nerve injury results from more than one factor. For example, a fracture may cause both compression and stretching of nearby nerves. Understanding the cause is essential for selecting the right treatment and preventing further damage.
What are the symptoms and signs of a nerve injury?
A nerve injury can produce symptoms that vary depending on the type of nerve affected and the severity of the damage. Symptoms appear because the injured nerve can no longer carry messages correctly between the brain, spinal cord, and body.
Common symptoms include:
Numbness: Loss of sensation in the skin or deeper tissues.
Tingling or “pins and needles”: Abnormal sensations that may come and go or persist.
Burning or sharp pain: Pain may be constant or triggered by touch or movement.
Weakness: Reduced muscle strength in the area served by the injured nerve.
Muscle wasting: Loss of muscle bulk if the injury is prolonged.
Coordination problems: Difficulty with fine motor skills or balance.
Recognizable signs during examination include:
Reduced reflexes: Slower or absent responses to reflex testing.
Skin changes: Altered temperature, color, or sweating in the affected area.
Loss of position sense: Inability to detect limb or joint position without looking.
Early identification of these symptoms and signs is important, as prompt treatment can reduce the risk of permanent nerve damage and improve recovery outcomes.
What are the types of nerve injuries?
Nerve injuries are classified based on the extent of damage to the nerve fibers and surrounding structures. The most widely used systems are the Seddon and Sunderland classifications.
Seddon’s classification includes three main types:
Neurapraxia: The mildest form, where the nerve is intact but electrical signaling is temporarily blocked. Recovery usually occurs within weeks to months.
Axonotmesis: The axon is damaged, but the surrounding connective tissue remains intact. The nerve can regenerate, but recovery takes months or longer.
Neurotmesis: The most severe form, where both the axon and surrounding structures are severed. Surgery is often required, and full recovery may not be possible.
Sunderland’s classification expands this into five degrees of injury, from mild conduction block (first degree) to complete nerve transection (fifth degree), offering a more detailed scale for diagnosis and treatment planning.
How is nerve injury diagnosis?
Diagnosing a nerve injury starts with a detailed medical history and physical examination. The doctor assesses symptoms, checks muscle strength, evaluates reflexes, and tests sensory function in the affected area.
Additional tests help confirm the diagnosis and measure the extent of damage:
Nerve conduction studies (NCS): Measure how quickly and effectively electrical signals travel along a nerve.
Electromyography (EMG): Records electrical activity in muscles to identify nerve or muscle dysfunction.
Imaging tests: MRI or ultrasound can detect nerve compression, swelling, or structural damage.
Quantitative sensory testing: Measures responses to touch, vibration, or temperature changes.
A combination of clinical evaluation and diagnostic tests ensures accurate identification of the nerve injury type and guides the choice of treatment. Early diagnosis increases the chances of successful recovery.
What happens when a nerve is injured?
When a nerve is injured, its ability to carry messages between the brain, spinal cord, and body is disrupted. This interruption can slow, alter, or completely block the electrical signals that control movement, sensation, and automatic functions.
Depending on the severity of the injury:
Temporary conduction block: The nerve’s structure remains intact, but swelling or compression interferes with signal transmission.
Axonal damage: The long fibers inside the nerve, called axons, are damaged, leading to degeneration of the section beyond the injury (Wallerian degeneration).
Complete transection: Both the axons and protective coverings are severed, preventing any signal transmission until surgical repair is attempted.
After injury, the body may attempt to repair the nerve. In mild cases, swelling subsides and signal conduction returns. In more severe cases, regeneration requires axonal growth, which occurs slowly, typically about 1 millimeter per day. If the nerve cannot regenerate or is not repaired, permanent loss of function may occur.
How do nerve pain and nerve damage manifest differently?
Nerve pain and nerve damage are related but not identical. Nerve pain refers to the discomfort caused by abnormal nerve signaling, while nerve damage describes the structural or functional injury to the nerve itself.
Nerve pain often presents as:
Burning, stabbing, or shooting sensations.
Tingling or “electric shock” feelings.
Pain triggered by light touch, cold, or movement.
Discomfort that may worsen at night or during rest.
Nerve damage produces broader effects, which may include:
Numbness or loss of sensation in the affected area.
Muscle weakness or paralysis.
Loss of coordination or reflexes.
Changes in skin temperature, color, or sweating.
A person can have nerve damage without pain, such as in complete sensory loss. Likewise, nerve pain can occur without visible structural damage, especially in early or mild cases. Distinguishing between the two helps determine treatment goals, relieving pain, restoring function, or both.
Which nerve types are most vulnerable?
All nerves can be injured, but certain types and locations are more at risk because of their position and function.
Peripheral nerves near joints: These nerves pass through tight spaces or around bony structures, making them prone to compression or stretching.
Examples include:
Ulnar nerve: Runs along the inside of the elbow and can be compressed in cubital tunnel syndrome.
Median nerve: Passes through the wrist in the carpal tunnel, often affected by repetitive hand movements.
Peroneal nerve: Wraps around the outside of the knee, vulnerable to crossing legs or knee injuries.
Related Content:
Large nerve networks:
Brachial plexus: Supplies the shoulder, arm, and hand. It can be stretched or torn during high-impact trauma or birth injuries.
Superficial sensory nerves: Located just under the skin, these are easily injured by cuts or blunt trauma.
Vulnerability depends on the nerve’s exposure, the surrounding anatomy, and the types of movements or pressures it experiences. Recognizing high-risk nerves allows for better prevention and early intervention.
How can a nerve repair itself?
A peripheral nerve has some ability to heal after injury, but the process is slow and depends on the extent of the damage. If the nerve’s outer protective covering remains intact, the inner fibers (axons) can regrow along the existing pathway. This regeneration usually happens at a rate of about 1 millimeter per day.
After injury:
Damaged sections of the axon beyond the injury site break down in a process called Wallerian degeneration.
Support cells, such as Schwann cells, clear debris and release growth factors that guide new axon growth.
The regenerating axon follows the remaining sheath toward its target muscle or sensory receptor.
Mild injuries, like neurapraxia, often recover fully without intervention. More severe injuries, such as axonotmesis, may take months to heal and require rehabilitation. In cases where the nerve pathway is disrupted, such as neurotmesis, natural repair is not possible without surgery.
Successful self-repair depends on early management, preventing further injury, and maintaining healthy surrounding tissues through therapy and care.
What are the nerve injury treatment options?
Treatment for a nerve injury depends on the type, location, and severity of the damage. The main goals are to restore nerve function, relieve symptoms, and prevent further injury.
Non-surgical treatments:
Rest and immobilization: Protects the injured nerve and reduces inflammation.
Physical and occupational therapy: Maintains joint movement, prevents muscle stiffness, and retrains muscles.
Medications: Pain relievers, anti-inflammatory drugs, or medicines for nerve pain such as gabapentin or duloxetine.
Splints or braces: Reduce pressure on the nerve and improve function.
Nerve blocks or electrical stimulation: Provide temporary pain relief and encourage nerve activity.
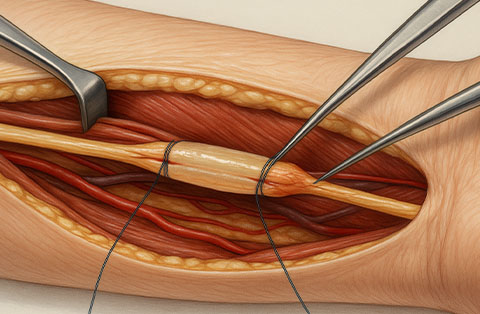
Surgical nerve treatments:
Nerve reconstruction surgery: A broad term that includes different surgical methods to restore the structure and function of a damaged nerve.
Nerve repair surgery: The ends of a cut nerve are carefully sutured together. This is done when the gap between the ends is short and can be closed without tension.
Nerve graft: A segment of healthy nerve from another part of the body is used to bridge a gap in the injured nerve when direct repair is not possible.
Nerve transfer surgery: A healthy nerve or one of its branches is redirected to restore function in an area where the original nerve cannot recover.
Neurolysis: The nerve is freed from surrounding scar tissue or other structures that are compressing it, allowing it to function more normally.
These surgical options are chosen based on the location, type, and severity of the nerve injury, as well as the time since the injury occurred. Early evaluation by a specialist can improve the chances of a good recovery.
When should brachial plexus injury be treated differently?
When should brachial plexus injury be treated differently?
A brachial plexus injury affects the network of nerves that control movement and sensation in the shoulder, arm, and hand. Because these nerves are vital for upper limb function, their injuries often require a different treatment approach than other peripheral nerve injuries.
Special treatment considerations are needed when:
The injury is severe: Complete tears (avulsions or ruptures) require early surgical intervention to restore nerve continuity and prevent permanent muscle loss.
Multiple nerves are involved: Damage to several branches can lead to complex weakness patterns, requiring a combination of nerve repair, nerve grafting, and nerve transfers.
There is no recovery after 3–6 months: Delayed improvement may mean the nerve cannot heal naturally, and surgical reconstruction becomes more urgent.
The injury is linked to trauma: High-energy accidents, such as motorcycle crashes, often cause severe stretching or tearing that will not recover without surgery.
Birth-related injuries (obstetric brachial plexus palsy): Infants may need early physiotherapy, and in some cases, surgery within the first year to restore function.
Early diagnosis is critical. Prompt referral to a specialist team experienced in brachial plexus surgery increases the chance of regaining useful arm and hand function.
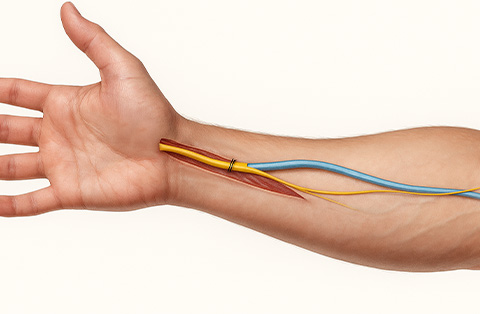
How are common compression injuries treated?
Compression injuries occur when a nerve is pressed by surrounding tissues such as muscles, ligaments, or bones. Common examples include carpal tunnel syndrome (median nerve compression at the wrist), cubital tunnel syndrome (ulnar nerve compression at the elbow), and peroneal nerve compression at the knee.
Treatment focuses on relieving pressure, restoring nerve function, and preventing further injury:
Non-surgical treatments:
Activity modification: Avoiding positions or movements that increase nerve pressure.
Splints or braces: Keeping the affected joint in a neutral position to reduce compression, especially at night.
Physical therapy: Stretching and strengthening exercises to reduce strain on the nerve.
Medications: Anti-inflammatory drugs or medications for nerve pain.
Corticosteroid injections: Used in some cases to reduce inflammation and swelling.
Surgical treatments:
Nerve decompression surgery: Removing or releasing the structure causing the pressure (e.g., cutting the ligament over the carpal tunnel).
Neurolysis: Freeing the nerve from scar tissue or adhesions that trap it.
Early intervention often prevents long-term nerve damage. Delaying treatment may lead to permanent weakness, numbness, or loss of coordination in the affected area.
What are the long-term outcomes and recovery expectations?
Long-term recovery after a nerve injury depends on the type, location, and severity of the damage, as well as how quickly treatment begins. Mild injuries, such as neurapraxia, often heal completely within weeks to months. More severe injuries, like axonotmesis or neurotmesis, may require many months of recovery or surgical intervention.
Factors influencing outcomes include:
Severity of the injury: Complete nerve transections have a lower chance of full recovery.
Time to treatment: Early diagnosis and management improve the likelihood of regaining function.
Patient age and health: Younger, healthier individuals generally heal faster.
Rehabilitation: Ongoing physical and occupational therapy helps maintain muscle strength, prevent stiffness, and improve coordination.
Possible long-term results:
Full restoration of movement and sensation in mild to moderate cases.
Partial recovery with residual weakness, numbness, or nerve pain in more severe cases.
Permanent loss of function if the nerve cannot regenerate or surgery is unsuccessful.
Recovery is typically slow, with nerve regrowth occurring at about 1 millimeter per day. Patience, consistent therapy, and close medical follow-up are essential for achieving the best possible outcome.
How does recovery progress after injury or surgery?
Recovery after a nerve injury or surgery follows a gradual process, as nerves heal and regrow slowly. The timeline depends on the severity of the injury, the type of treatment, and the patient’s overall health.
Typical stages of recovery:
Initial healing (first weeks): Swelling and inflammation reduce, and pain may lessen. In cases of mild injury, nerve conduction can begin to improve quickly.
Regeneration phase (weeks to months): Damaged axons regrow at a rate of about 1 millimeter per day. Sensation and movement gradually return, starting from the area closest to the injury site.
Rehabilitation phase (months to years): Physical and occupational therapy strengthen muscles, restore coordination, and retrain the nervous system to use regained function.
After surgery, recovery often includes:
Protection: Immobilization or splinting to safeguard the repair.
Gradual mobilization: Controlled exercises to prevent stiffness without stressing the repair.
Sensory re-education: Techniques to help the brain interpret new or returning nerve signals.
Full recovery can take several months to years. Some patients regain complete function, while others may have lasting weakness, numbness, or nerve pain despite optimal treatment. Regular follow-up ensures progress is monitored and therapy is adjusted as needed.
When is nerve damage permanent and recovery unlikely?
When is nerve damage permanent and recovery unlikely?
Nerve damage becomes permanent when the injury is too severe for the nerve to regenerate or when repair is delayed beyond the window for meaningful recovery. In these cases, the affected muscles, sensory areas, or both lose function for good.
Situations where recovery is unlikely include:
Complete nerve transection without repair: If a severed nerve is not surgically reconnected in time, the pathway for regeneration is lost.
Severe neurotmesis: When both the axon and its protective coverings are destroyed, even surgery may not restore function if the damage is extensive.
Prolonged denervation: If a muscle remains without nerve supply for more than 12–18 months, it may undergo irreversible atrophy.
Chronic compression injuries: Long-standing nerve pressure, as in untreated carpal tunnel syndrome, can cause lasting loss of sensation and strength.
Underlying disease damage: Conditions like advanced diabetes or certain autoimmune disorders can cause irreversible nerve fiber loss.
Early evaluation and intervention are key to preventing permanent deficits. Once irreversible damage has occurred, treatment focuses on managing symptoms, preventing secondary complications, and maximizing remaining function.
Frequently Asked Questions
How do underlying health conditions affect nerve injury risk and healing?
Chronic conditions like diabetes, autoimmune diseases, and vascular disorders increase the risk of nerve injury by reducing blood flow, causing inflammation, or damaging nerve fibers. These conditions can also slow healing, as poor circulation and impaired cellular repair limit regeneration. Effective management of the underlying disease improves recovery chances.
What home-based care tips support nerve recovery?
Home-based nerve recovery includes gentle stretching, regular low-impact exercise, and a balanced diet rich in vitamins B and E for nerve health. Protect the injured area from further stress, maintain good posture, and follow prescribed therapy routines. Adequate rest and avoiding repetitive strain support healing and prevent additional damage.
How can patients prevent nerve injury?
Patients can prevent nerve injury by maintaining good posture, using ergonomic workstations, and taking regular breaks during repetitive tasks. Wearing protective gear during sports or high-risk activities reduces trauma risk. Managing chronic conditions, avoiding prolonged pressure on joints, and practicing safe lifting techniques also help protect nerves from damage.
When should someone seek medical help for nerve pain or injury?
Seek medical help for nerve pain or injury if symptoms appear suddenly, worsen quickly, or include weakness, numbness, or loss of coordination. Immediate evaluation is essential after trauma, deep cuts, or electric shocks. Persistent nerve pain, burning sensations, or unexplained tingling also require prompt medical assessment to prevent lasting damage.
Which nerve injury causes hoarseness of voice?
Hoarseness of voice can result from injury to the recurrent laryngeal nerve, a branch of the vagus nerve. This nerve controls most of the muscles in the voice box. Damage may occur during neck or chest surgery, trauma, or from tumors, leading to vocal cord weakness and altered voice quality.
Can nerve injury cause ALS?
Nerve injury does not cause amyotrophic lateral sclerosis (ALS). ALS is a progressive neurodegenerative disease affecting motor neurons, with causes linked to genetic and environmental factors. While nerve injuries can cause weakness, numbness, or pain, they do not trigger ALS. However, both conditions may share some overlapping early symptoms.