Struggling with pain, tingling, or weakness from a pinched nerve? Learn how to identify nerve compression syndrome early and explore effective treatments to prevent lasting nerve damage.
Nerve compression syndrome happens when a nerve is pressed or “pinched” by nearby tissues, leading to pain, numbness, or weakness, usually in the hands, arms, legs, or feet.
In this guide, we’ll explain what nerve compression syndrome is, what causes it, how to recognize symptoms early, and which treatment options can help relieve pressure and restore function.
What Is Nerve Compression Syndrome?
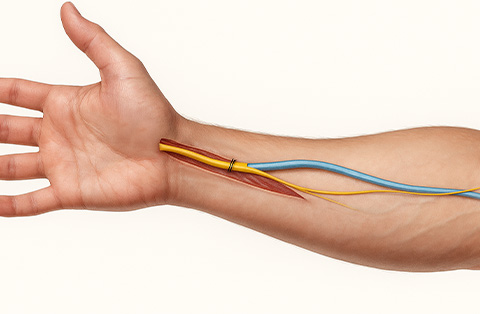
Nerve compression syndrome, also called entrapment neuropathy is a condition where a nerve is compressed or pinched by surrounding tissues. These tissues may include muscles, tendons, ligaments, bones, or cartilage. The pressure disrupts normal nerve function, often causing pain, numbness, tingling, or weakness in the affected area.
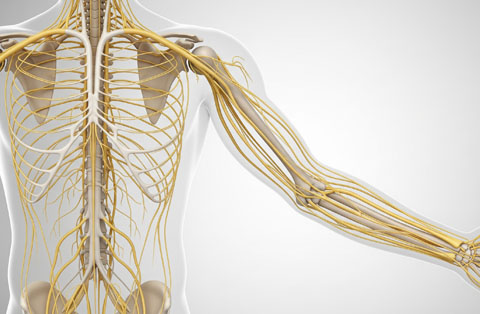
This condition typically affects peripheral nerves (the nerves outside the brain and spinal cord). When these nerves are compressed, signals between the brain and the body can become impaired. The location and severity of compression determine the type and intensity of symptoms.
Nerve compression syndrome can occur in various parts of the body, especially in areas where nerves travel through narrow spaces and lack soft tissue protection. Common examples include carpal tunnel syndrome (wrist), cubital tunnel syndrome (elbow), and tarsal tunnel syndrome (ankle).
The condition may develop gradually due to repetitive movements or posture, or it may result from an injury, anatomical variation, or underlying disease. Early diagnosis and treatment are essential to prevent permanent nerve damage.
How Does It Affect the Nerve?
When a nerve is compressed, the pressure interferes with its normal function in several ways. First, the physical pressure restricts blood flow (called ischemia) to the nerve. Without adequate oxygen and nutrients, the nerve fibers can’t transmit signals properly.
Compression also causes irritation and inflammation of the nerve sheath, the protective covering around the nerve. This leads to abnormal electrical activity in the nerve, which can trigger symptoms like pain, tingling, or burning sensations.
If the compression continues, it may damage the myelin sheath (the insulating layer around nerve fibers). In more severe or prolonged cases, the underlying axon (the core of the nerve cell) may also be injured. This can result in muscle weakness, reduced reflexes, and even long-term sensory or motor deficits.
The severity and duration of compression determine how reversible the damage is. In early stages, symptoms may come and go. But without treatment, the nerve may suffer permanent damage, especially if the cause of compression isn't removed.
How Does a Nerve Under Compression Cause Entrapment Neuropathy?
Entrapment neuropathy occurs when a nerve is chronically compressed or trapped in a confined anatomical space. This prolonged pressure disrupts both the structure and function of the nerve. Over time, the nerve becomes inflamed and damaged, leading to neuropathic symptoms.
The compression first affects the nerve’s ability to conduct electrical signals. As pressure builds, the myelin sheath (responsible for fast signal transmission) is damaged. This results in slower or blocked communication between the nerve and muscles or skin.
If left untreated, the continued pressure may lead to degeneration of the axon itself. This causes more severe symptoms like persistent numbness, muscle wasting, and loss of coordination or strength.
Entrapment neuropathy often develops in high-risk sites where nerves pass through tight spaces or near rigid structures, such as the wrist (carpal tunnel) or elbow (cubital tunnel). The combination of mechanical stress, inflammation, and reduced circulation creates a cycle of ongoing nerve injury.
What Happens When a Peripheral Nerve Is Compressed?
When a peripheral nerve is compressed, its ability to transmit sensory and motor signals is disrupted. This leads to symptoms like pain, numbness, tingling, or weakness in the area the nerve supplies.
Initially, compression reduces blood flow to the nerve, causing local ischemia and irritation. The nerve's protective myelin sheath may become damaged, affecting signal speed and accuracy. As the compression continues, the nerve may start sending abnormal signals or fail to send signals altogether.
Depending on the location and severity, symptoms may be intermittent or constant. For example, compression in the wrist can cause hand tingling, while compression near the spine may affect an entire limb.
In chronic cases, the underlying nerve fibers (axons) can degenerate. This can result in muscle atrophy, reduced reflexes, and long-term sensory loss. Early intervention is key to preventing permanent dysfunction of the peripheral nervous system.
Which Parts of the Body Can Be Affected by This Syndrome?
Nerve compression syndrome can affect almost any part of the body where a peripheral nerve passes through a narrow or restricted space. The most commonly affected areas are the limbs—especially joints—where nerves are more likely to become compressed by bones, tendons, or muscles during movement or repetitive use.
Upper Extremities
The upper limbs are the most frequent site of nerve compression syndromes. Common examples include:
Wrist (Carpal Tunnel Syndrome): Compression of the median nerve causes numbness and tingling in the thumb, index, and middle fingers.
Elbow (Cubital Tunnel Syndrome): Ulnar nerve compression results in pain and tingling in the ring and little fingers.
Shoulder/Neck (Thoracic Outlet Syndrome): Compression of the brachial plexus leads to pain, weakness, and numbness in the arm and hand.
Related Content: Upper Extremity Reconstruction
Lower Extremities
Although less common than in the arms, compression can occur in the legs as well:
Ankle (Tarsal Tunnel Syndrome): The tibial nerve is compressed, causing burning, tingling, or numbness in the sole of the foot.
Fibular Head (Common Peroneal Nerve Compression): This can cause foot drop, numbness, or weakness on the outer side of the leg and top of the foot.
Trunk and Spine
Spinal Nerve Roots (Radiculopathy): Herniated discs or spinal stenosis can compress nerve roots as they exit the spine, causing radiating pain, numbness, or weakness in the arms or legs, depending on the level affected.
In each case, the location of symptoms reflects the function and path of the specific compressed nerve.
What Are the Symptoms of Nerve Compression and a Pinched Nerve?
The symptoms of nerve compression and a pinched nerve can vary depending on which nerve is affected, how long it's been compressed, and how severe the compression is. In most cases, symptoms develop gradually and may worsen over time without treatment.
What Are the Symptoms of Nerve Compression Syndrome (General)?
General signs of nerve compression syndrome include:
Pain near the site of compression, often radiating along the nerve path
Tingling or “pins and needles” sensations (paresthesia)
Numbness in the skin supplied by the compressed nerve
Muscle weakness in the affected area
Loss of coordination or reduced fine motor control
These symptoms usually appear in the hands, arms, feet, or legs, depending on the location of the compressed nerve. They may be worse during or after activity and may improve with rest—at least in the early stages.
What Are the Symptoms of a Pinched Nerve Specifically?
A pinched nerve typically causes more localized and mechanical symptoms, including:
Sharp, shooting pain or a burning sensation along the nerve path
Localized muscle weakness, such as a weak grip or foot drop
Symptoms that worsen with certain movements, like bending the wrist or elbow
Numbness or tingling that comes and goes, often triggered by posture or activity
Pinched nerves in the spine may cause radiculopathy, where symptoms radiate down an arm or leg. In contrast, a pinched nerve in the wrist or elbow may affect hand function directly.
How Does Neuropathy Present in a Compressed Nerve?
Over time, chronic compression can lead to neuropathy, which refers to lasting nerve damage. Signs of neuropathy from prolonged compression include:
Persistent numbness or tingling
Chronic burning pain
Muscle atrophy, especially in the hands or feet
Decreased reflexes and impaired sensation
Once neuropathy develops, recovery is slower and may not be complete, even after compression is relieved. Early detection and intervention are key to preventing permanent damage.
What Causes Nerve Compression?
Nerve compression occurs when external pressure disrupts the function of a peripheral nerve. This pressure can come from surrounding tissues, such as muscles, bones, ligaments, or tendons—or from structural changes in the body. The causes are often multifactorial and can be either acute or chronic.
How Do Structural or Anatomical Factors Lead to Compression?
Some individuals are born with anatomical variations that make certain nerves more vulnerable to compression. These may include:
Narrow passageways through which nerves must travel
Bone spurs or thickened ligaments from arthritis
Cysts or tumors that press against nearby nerves
Postural abnormalities that change joint mechanics
These structural issues can limit space around a nerve, increasing the risk of entrapment even during routine movements.
Can Overuse or Repetitive Stress Pinch a Nerve?
Yes. Repetitive motion or prolonged positioning is a common cause of nerve compression. Examples include:
Typing or using a mouse for long periods (risking carpal tunnel syndrome)
Leaning on the elbows frequently (risking cubital tunnel syndrome)
Frequent bending of the wrist, knee, or ankle during work or sports
Over time, these activities cause inflammation and swelling, which can compress nearby nerves.
What Systemic Conditions Contribute to Syndrome-Related Nerve Compression?
Certain medical conditions can increase the likelihood of developing nerve compression syndromes:
Diabetes, which increases susceptibility to nerve damage and swelling
Rheumatoid arthritis, which causes joint inflammation and deformity
Thyroid disorders, which can lead to tissue thickening
Obesity, which increases mechanical stress on joints and nerves
Pregnancy, due to fluid retention and hormonal changes that affect connective tissues
In some cases, a combination of mechanical stress and systemic disease causes or worsens the compression. Identifying the underlying cause is essential to guiding treatment and preventing recurrence.
How Is Nerve Compression Syndrome Diagnosed?
Diagnosing nerve compression syndrome involves a detailed clinical evaluation, supported by diagnostic tests that confirm the site and severity of nerve involvement. The goal is to identify which nerve is compressed, what’s causing the compression, and how much damage has occurred.
What Tests and Clinical Exams Identify a Compressed Nerve?
A healthcare provider will begin with a physical examination and detailed medical history. Key steps include:
Sensory testing: to detect areas of numbness or tingling
Muscle strength testing: to assess weakness or muscle atrophy
Reflex testing: to identify reduced or absent reflexes
Provocative maneuvers: such as Tinel’s sign or Phalen’s test for carpal tunnel syndrome
These tests help localize the problem and differentiate between nerve compression and other conditions like vascular disorders or systemic neuropathy.
When Are Imaging or Electrophysiology Studies Used?
If symptoms persist or the diagnosis is unclear, further testing may be required:
Electromyography (EMG) and nerve conduction studies (NCS)
These measure how well electrical signals travel through the nerve. They confirm the diagnosis, localize the site of compression, and determine the severity of nerve damage.Ultrasound
High-resolution ultrasound can visualize the compressed nerve and surrounding tissues in real-time, especially useful in dynamic conditions or small anatomical spaces.Magnetic Resonance Imaging (MRI)
MRI helps identify structural causes of compression, such as disc herniation, tumors, or soft tissue abnormalities.X-rays
These may be used to detect bone spurs, fractures, or joint deformities contributing to nerve compression.
A clear diagnosis allows for appropriate treatment planning (whether conservative or surgical) and helps prevent permanent nerve injury.
What Are Treatment Options for Nerve Compression and Entrapment Neuropathy?
Treatment for nerve compression and entrapment neuropathy depends on the severity of symptoms, the cause of compression, and how long the nerve has been affected. The main goal is to relieve pressure on the nerve, reduce inflammation, and prevent long-term damage.
Which Conservative Treatments Help Relieve a Pinched Nerve?
In most cases, mild to moderate nerve compression can be managed without surgery. Common non-surgical treatments include:
Activity modification: Avoiding repetitive motions or prolonged positions that aggravate symptoms
Bracing or splinting: Using wrist, elbow, or ankle supports to reduce movement and protect the nerve
Physical therapy: Stretching and strengthening exercises to improve posture and reduce tension on the nerve
Anti-inflammatory medications: NSAIDs can help reduce swelling around the nerve
Steroid injections: In some cases, corticosteroids may be injected near the nerve to decrease inflammation
These approaches are typically tried for several weeks to months. Early intervention improves the chance of full recovery.
When Is Surgical Decompression Needed for the Compressed Nerve?
Nerve surgery may be recommended if:
Symptoms persist or worsen despite conservative treatment
Nerve function is progressively declining (e.g., increasing weakness or numbness)
Imaging or nerve studies show severe compression or damage
Surgical decompression involves removing or releasing the tissue that’s pressing on the nerve. The specific procedure depends on the location, for example, carpal tunnel release at the wrist or ulnar nerve transposition at the elbow. In some cases, damaged nerve tissue may need repair or reconstruction.