Struggling with dry eye after cataract surgery? Learn why it happens, how long it lasts, and the proven treatments that restore comfort and protect your vision.
Dry eye after cataract surgery happens when the tear film becomes unstable, leaving the eye surface irritated and less comfortable. It’s one of the most common complaints patients face during recovery.
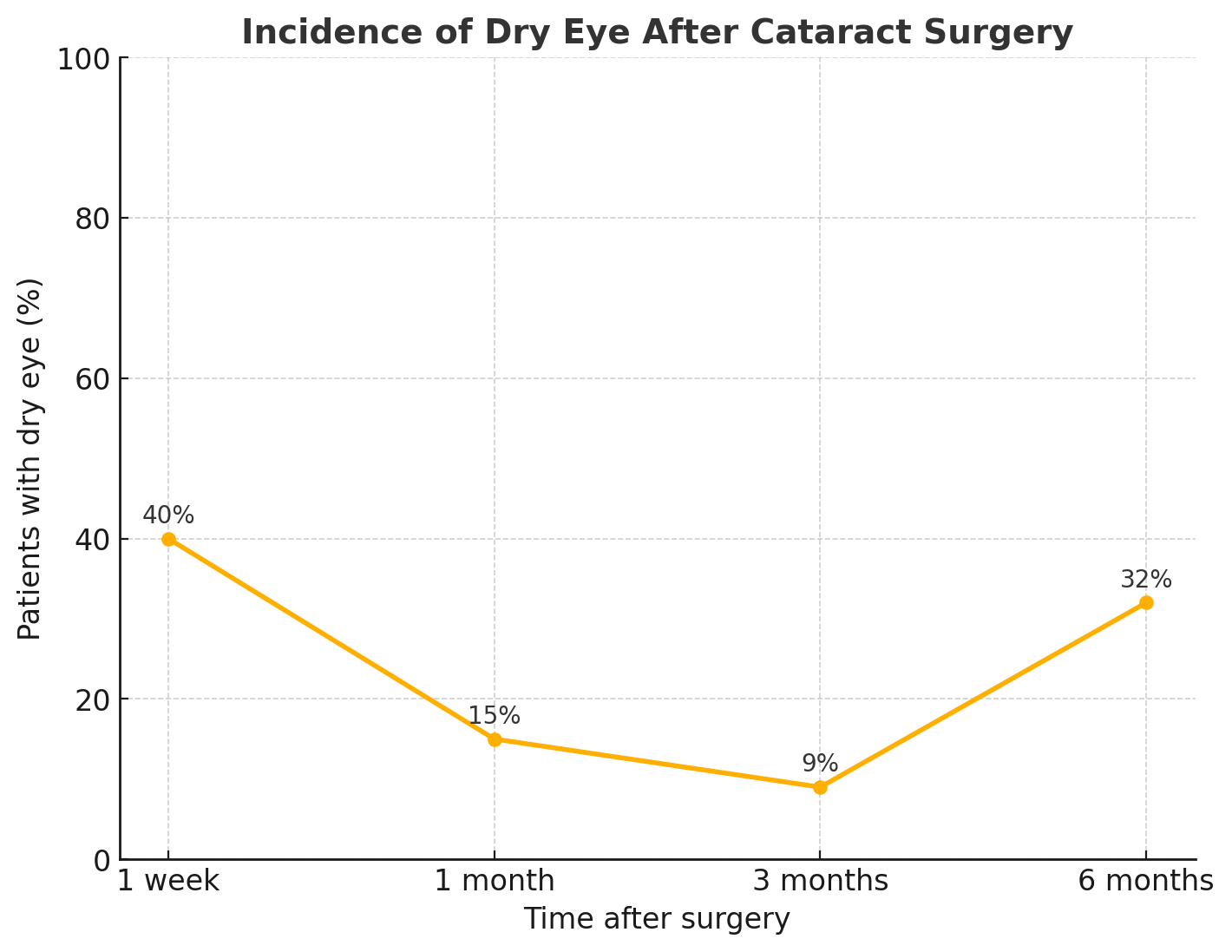
Research shows that up to 40% of patients develop dry eye symptoms in the first weeks after surgery, although most improve within a few months. Understanding why this happens and how to manage it is key to ensuring clear vision and a smooth recovery.
In this article, we’ll explain what cataracts and dry eye syndrome are, why dry eye can occur after cataract surgery, how common it is, the risk factors involved, and the best treatments and prevention strategies to protect your eye health.
What are cataracts?
A cataract is the clouding of the eye’s natural lens. The lens normally helps focus light on the retina, creating clear vision. When proteins in the lens break down and clump together, the lens becomes cloudy, leading to blurred or hazy vision.
Cataracts develop slowly and often affect both eyes, although one may be worse than the other. They are most common with aging, but they can also result from eye injuries, certain medications, or underlying conditions like diabetes.
Cataract Symptoms:
Blurred or dim vision
Glare or halos around lights
Difficulty seeing at night
Faded colors
Frequent changes in glasses prescriptions
If left untreated, cataracts progress and cause significant vision loss. Cataract surgery, which removes the cloudy lens and replaces it with an artificial intraocular lens, is the only effective treatment.
What is dry eye syndrome?
Dry eye syndrome is a condition where the eyes don’t produce enough tears or the tears evaporate too quickly. Tears are essential for keeping the surface of the eye moist, smooth, and protected from irritation.
When tear quantity or quality is poor, the eye surface becomes dry and inflamed. This causes discomfort and may interfere with vision.
Ocular surface diseases prevent the eyes from producing enough tears or the right quality of tears.
What are the symptoms of dry eye syndrome?
Burning, stinging, or scratchy sensation
Redness and irritation
Blurred vision that improves with blinking
Sensitivity to light
Feeling of “something in the eye”
Dry eye syndrome can result from aging, hormonal changes, certain medications, autoimmune diseases, or environmental factors like wind and screen use. In severe cases, it increases the risk of eye infections and damage to the cornea.
Do cataracts cause dry eyes?
Cataracts do not directly cause dry eye syndrome. A cataract is a clouding of the eye’s lens, while dry eye involves the tear film and surface of the eye. These are two separate conditions that affect vision differently.
However, people with cataracts are often older, and age is a major risk factor for both cataracts and dry eye disease. In this way, cataracts and dry eye frequently appear together, but one does not cause the other.
Some patients may notice eye discomfort or dryness while living with cataracts. This is usually due to age-related tear film changes, existing dry eye disease, or other health conditions rather than the cataract itself.
The stronger link comes after surgery: cataract surgery can temporarily worsen or trigger dry eye symptoms, which is why many patients associate the two.
What causes dry eyes after cataract surgery?
Dry eyes after cataract surgery occur because the procedure temporarily disrupts the ocular surface and tear film balance. Several mechanisms contribute:
Corneal nerve disturbance: Small incisions made during surgery cut some of the corneal nerves that signal tear production. This reduces reflex tearing and causes surface dryness until the nerves heal.
Inflammatory response: Surgery triggers local inflammation, which can alter tear film stability and increase evaporation.
Tear film instability: Changes to the corneal surface affect how tears spread evenly across the eye, leading to patches of dryness.
Pre-existing vulnerability: Many patients already have age-related tear gland decline or mild dry eye before surgery, which surgery can aggravate.
Medication effects: Postoperative drops, especially those with preservatives, may irritate the eye surface and worsen dryness.
These factors usually cause temporary symptoms. In most cases, the eye surface heals and tear function improves over weeks to months, but some patients with underlying dry eye disease may experience longer-lasting effects.
Do all patients experience dry eye syndrome after cataract surgery?
Not every patient develops dry eye syndrome after cataract surgery. Many experience at least temporary dryness or irritation in the early weeks, but the severity and duration vary widely.
Studies show a high incidence of dry eye symptoms immediately after surgery, but most cases improve within 3 to 6 months. Some patients never notice discomfort, while others with pre-existing dry eye disease may find their condition worsens or persists longer.
Key factors that influence who develops dry eye include:
Age and hormonal status
History of dry eye or autoimmune disease
Extent of pre-existing tear film instability
Surgical technique and incision size
Frequency and type of postoperative eye drops used
So, while temporary dryness is common, lasting dry eye syndrome is not universal. Patients with underlying risk factors are more likely to experience significant or prolonged symptoms.
Facts on incidence and persistence of dry eye after cataract surgery
A meta-analysis combining 9 studies (775 patients without prior dry eye) found that 37.4% (95% CI 22.6–52.3%) of patients developed dry eye disease (DED) after cataract surgery.
One prospective study reported that 42% of eyes showed dry eye signs at 1 week, but this dropped to 15% at 1 month and 9% at 3 months postoperatively.
In phacoemulsification-only cases, the incidence 7 days after surgery was about 9.8%, per a PLOS One article.
Another study of patients undergoing phacoemulsification found incidence of 38% at day 7, decreasing to 8% at 1 month.
What’s the treatment for post-cataract surgery dry eye syndrome?
Care focuses on four goals: restore the tear film, calm inflammation, stabilize eyelids, and protect the cornea.
1) Stabilize the tear film
Use preservative-free lubrication to replenish aqueous volume and reduce friction.
Add lipid-support options when meibomian gland dysfunction drives evaporation.
Improve eyelid function with gentle hygiene and heat to normalize oil flow.
2) Reduce ocular surface inflammation
Short courses of topical corticosteroids help break acute flare-ups.
Immunomodulators (e.g., cyclosporine or lifitegrast) address T-cell inflammation and improve tear quality over weeks.
Treat coexisting allergy or blepharitis to remove inflammatory triggers.
3) Retain tears longer
Punctal occlusion is considered when aqueous deficiency persists despite drops.
Humidified environments and blink training lower evaporative loss, especially during screen use.
4) Protect and repair the surface
Osmoprotective, hyaluronate-rich, or trehalose-based formulas support epithelial healing.
In moderate–severe disease, autologous serum or platelet-rich tears can promote regeneration.
Bandage or scleral lenses shield the cornea when pain or exposure is significant.
5) Optimize medications and comorbidities
Switch postoperative drops to preservative-free versions when possible.
Review systemic drugs that can cause dry eye and coordinate changes with the prescribing doctor.
Address systemic drivers such as thyroid disease, diabetes, or autoimmune conditions.
6) Triage and timeline
Expect the peak of symptoms in the first month, then gradual improvement.
Reassess at 4–6 weeks; escalate therapy if vision, staining, or symptoms persist.
Refer to a dry eye specialist when symptoms remain beyond 3 months or corneal damage appears.
7) Outcomes to set expectations
Most patients improve with layered therapy and time.
Those with pre-existing dry eye or strong evaporative components may need long-term maintenance.
Early treatment protects surgical outcomes and optimizes visual quality from the new intraocular lens.
Learn more about dry eye syndrome self care tips.
How to prevent dry eyes after cataract surgery?
Prevention focuses on preparing the ocular surface before surgery and protecting it during recovery. Addressing tear film health early lowers the chance of persistent symptoms.
Before surgery
Screen for dry eye disease: Detect tear instability, meibomian gland dysfunction, or inflammation and manage them prior to surgery.
Stabilize the tear film: Start artificial tears or anti-inflammatory drops if baseline dryness is present.
Treat eyelid disease: Manage blepharitis or meibomian gland dysfunction to optimize the tear film before surgery.
During surgery
Minimize incision size: Small, precise cuts reduce corneal nerve damage and preserve tear reflex pathways.
Use protective techniques: Surgeons may reduce exposure time and avoid unnecessary manipulation of the ocular surface.
After surgery
Follow prescribed regimen: Use preservative-free drops to avoid further irritation.
Limit screen strain: Frequent blinking and breaks prevent excessive evaporation.
Protect from environment: Avoid wind, smoke, and low humidity that worsen evaporation.
Adhere to follow-ups: Regular checkups allow early treatment if dryness develops.
Preventive steps don’t eliminate the risk completely, but they significantly reduce severity and improve recovery comfort.
When should you see an eye doctor?
Most patients feel mild dryness after cataract surgery, but certain signs mean you should seek medical evaluation.
See your eye doctor if you notice:
Severe dry eye, burning, or irritation that doesn’t improve with lubricating drops
Blurred vision that lasts beyond the first weeks of recovery
Sensitivity to light that interferes with daily activities
Sharp pain, sudden vision changes, or worsening redness
Mucus discharge, swelling, or signs of infection
Symptoms that remain beyond 3 months after surgery
Routine follow-ups are also essential:
Your scheduled postoperative visits allow the surgeon to check corneal healing and tear film stability.
Even without severe symptoms, reporting dryness helps your doctor adjust medications or add treatment before problems worsen.
Prompt attention protects the health of your eye surface, ensures clear visual recovery, and lowers the risk of long-term dry eye disease.
Frequently Asked Questions
Is dry eye after cataract surgery permanent?
Dry eye after cataract surgery is usually temporary. Most cataract patients notice symptoms in the first weeks, which improve as the eye surface heals. A minority with pre-existing dry eye disease may continue to experience dryness long term, but early treatment and follow-up reduce the risk of permanent discomfort.
Will dry eye syndrome make my eyes take longer to heal after cataract surgery?
Yes. Dry eye syndrome can slow visual recovery following cataract surgery because an unstable tear film affects corneal healing and clarity. Most patients still recover well, but untreated dryness may delay comfort and sharpness. Managing dry eye early supports smoother healing, clearer vision, and better long-term results after the procedure.
How long does dry eye last after cataract surgery?
Dry eye after cataract surgery may last a few weeks to several months. Symptoms are often most noticeable during the first month and gradually improve as nerves heal. For some, surgery may uncover pre-existing dry eye disease, making symptoms persist longer. Proper treatment helps shorten recovery and improve eye comfort.
How often should I use lubricating eye drops after cataract surgery?
Lubricating eye drops are typically used several times daily after cataract surgery, especially in the first few weeks. Frequency depends on symptom severity and your doctor’s advice. Some patients may need drops every few hours, while others only two to three times a day. Always follow your surgeon’s instructions.
What happens if I don't use my eye drops after cataract surgery?
Skipping prescribed eye drops after cataract surgery can slow healing, increase inflammation, and raise infection risk. Without lubrication, dry eye symptoms may worsen, causing discomfort and blurred vision. Anti-inflammatory or antibiotic drops also protect the eye. Not using them may compromise surgical results and long-term vision quality.
Which symptoms are abnormal after cataract surgery?
After cataract surgery, mild dryness, light sensitivity, or blurred vision are normal in early recovery. Abnormal symptoms include severe or increasing eye pain, sudden vision loss, marked redness, swelling, or discharge. These may signal infection, inflammation, or complications. Any unexpected or worsening symptoms should be reported to your eye doctor immediately.